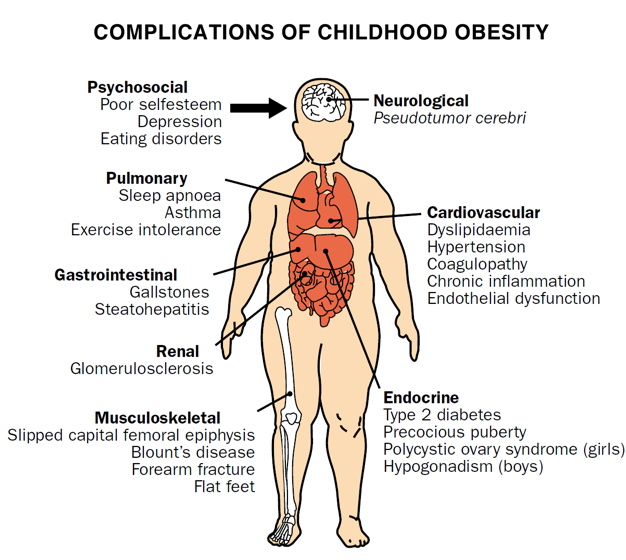
Childhood obesity and adolescent obesity is linked with many serious health issues in adulthood. Unfortunately, there is little evidence that preventive measures such as lifestyle interventions and pharmacological treatments are effective. There are several surgical procedures for children and adolescents but the long term effects remain uncertain.
Researchers from University College of Gjovik and the University of Oslo, Norway in a paper “Bariatric surgery for obese children and adolescents: A review of the moral challenges” concluded that surgery on children’s healthy organs to discipline their eating behavior in order to help them to be socially acceptable or to compensate for poor parenting is ill advised. There needs to be more evidence on outcomes and risk factors. There also needs to be a valid consent or assent.
In making a decision on bariatric surgery for children and adolescents, parents need to look at the moral implications with regard to values, viewpoints and arguments before they make the decision to go forward.
Long Term Outcomes and Benefits of Bariatric Surgery for Children
There is little evidence on the benefits of bariatric surgery on youngsters. The overwhelming research has been on adults and those results don’t necessarily generalize to a children and adolescents. If, after 100 – 150 procedures there are few complications then it might be permissible to perform this procedure, but only in specialized, high volume centers where the doctors have plenty of experience.
Much consideration needs to be given to how this procedure might affect psychological and social development. Few studies address these issues. The other moral consideration is informed consent. Should a parent make the decision for a child, or is a child or adolescent mature enough to have a say? Surgery should not replace self discipline.
Studies show that one third of obese adults were sexually abused as children. So as part of the assessment process for children and adolescents, this should be addressed.
Preconceptions on Bariatric Surgery for Youth
Overweight children and adolescents are often the target of discrimination and prejudice. And medical practitioners are known to also discriminate against the obese, by assuming they are ill prepared to take care of themselves. So, few referrals are made for surgery among this population. But should this social problem be addressed with surgery anyway?
Bariatric surgery poses particular questions for minors because it uses medical interventions to alter everyday behavior when there are other solutions available such as dieting, exercising, and cognitive behavioral therapy that pose no risk to healthy organs in the body. Also this surgery does not address the many unknown causes of obesity.
In conclusion these researchers posed the following questions that need to be addressed when making a decision such as bariatric surgery for a child or adolescent:
- Who to operate on
- When to do it
- Who is to decide
- How to decide
- Who is to operate
- How best to prepare
- How to follow-up
And the most important question would be how to generate more high quality evidence in a morally acceptable manner.
I would love to know your option on this topic of Childhood Obesity and Bariatric Surgery. Please Comment!