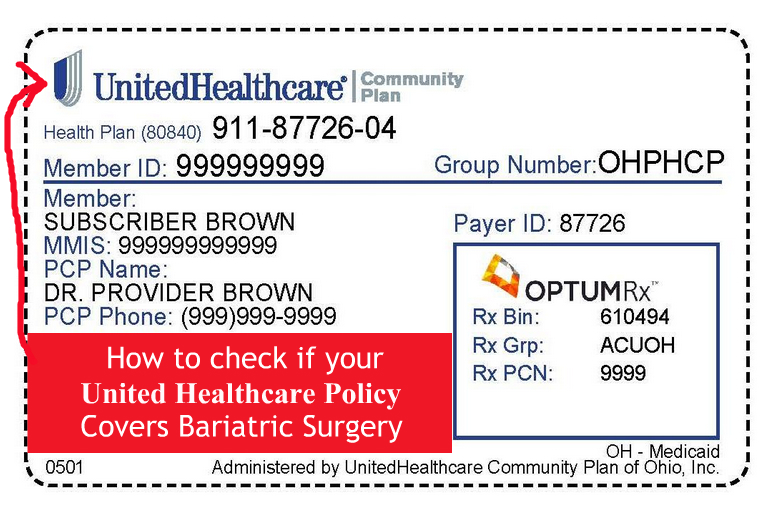
United Healthcare Insurance
What Does United Healthcare Cover For Bariatric Surgeries
There are many excluded coverages for weight loss surgery with United Healthcare. However, there are several plans that will cover the surgery. There are some states that demand insurance companies to pay for weight loss surgery. Thus, if your policy does not include, your state may mandate the coverage.
What Criteria Must A Person Have Before United Healthcare Pays For The Bariatric Surgery
The criteria below will need to be met for coverage to be approved:
- Class 3 Obesity or 40+BMI (Body Mass Index)
- Class 2 Obesity of 35+BMI with any of the three following conditions:
– Cardiovascular disease
– Life-threatening cardiopulmonary or severe sleep apnea
– Type 2 diabetes
MARYLAND REQUIREMENTS FOR COMPLETELY INSURED POLICIES
- 40+ BMI without any health conditions
- 35+BMI with the following conditions
– Hypertension
– Diabetes
– Sleep apnea
– Cardiopulmonary condition
– Life-threatening weight-induced medical condition - Proof that you have done diets but were not successful – Weight Watchers, Jenny Craig, etc. – for the last two years:
– Participated in 1 organized diet platform for six successive months
– Participated in 2 organized diet platforms for three successive months - At least 18 years of age or more
What Kind Of Weight Loss Surgeries Does United Healthcare Covers
- Biliopancreatic bypass
- Duodenal switch
- Gastric bypass
- Gastric Sleeve Procedure
- Lap Adjustable Gastric Bands
- Vertical banded gastroplasty
For adolescents
- Gastric bypass
- Gastric sleeve
- Lap gastric bands
Lap Gastric Band Fills: Are They Covered
United Healthcare does cover the lap gastric band fills for patients who undergo the Realize Band surgery or the Lap Band surgery.
What Weight Loss Procedures Does United HealthCare Not Cover
- Gastric electrical stimulation
- Mini-gastric bypass
- ROSE, StomaphyX, TOGA
Is a Second Surgery Allowed If The Lap Band Fails (Revisions)?
Assuming you have the same conditions from the first procedures, then yes a second surgery will be covered.
What If You Do Not Lose Weight?
If there are complications from the surgery, United Healthcare will cover all procedures and hospital stay.
Is A Center of Excellence Needed?
Nope. However, if you choose an in-network doctor, you can save yourself money – no out of pocket expenses.
Contact Information For United Healthcare
The contact information for United Healthcare varies by state.