Patients Denied Insurance for Bariatric Surgery Face Increased Health Risks
Patients Denied Insurance for Bariatric Surgery Face Increasing Health Risks
When health insurers deny insurance coverage for bariatric surgery to eligible patients, the likelihood of these patients developing additional obesity-related conditions and diseases rises significantly year after year, according to a new study.
It is widely accepted that bariatric surgery can often reduce or even eliminate any existing conditions, or co-morbidities. And it is also well-known that even though the patients’ body mass index (BMI) remains about the same, any illnesses, or comorbidities that exist can worsen, the study showed.
Researchers evaluated patients’ medical records for the period from 2001 to 2007, comparing the histories of patients who had laparoscopic gastric bypass with those of patients who were medically eligible but were denied insurance coverage for the procedure.
About 30% of the patients who met criteria for weight loss surgery were not able to have the surgery because their insurance carriers found their claims unsupportable for various reasons, or the claims were simply denied.
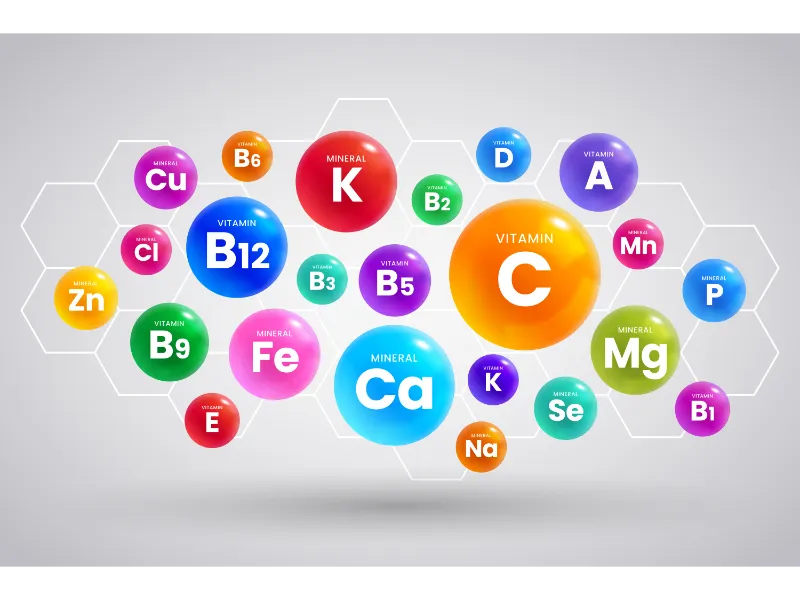
Both groups of patients involved in the study had a BMI average of about 48. Co-morbidity rates for both the surgery-accepted and the denial group were, respectively: diabetes, 24% and 20%; gastroesophageal reflux disease, 49% and 62%; sleep apnea, 22% and 20%; lipid disorders, 24% and 34%; and hypertension, 43% and 51%.
Medical results from a three-year follow up exam showed that the surgical group patients had lowered their BMI to 30.5%, and less than 1% had experienced any new conditions related to obesity. In contrast, the majority of the patients in the denial group had developed a variety of obesity-related medical conditions, despite the fact that their BMI had basically stayed the same.
Researchers emphasized the wide gap between the two groups in terms of disease development, calling the disparity especially significant. When comparing the surgical group to the surgery-denied group, respectively: 0.3% vs. 9.2% developed diabetes; 0.6% vs. 19.4% developed gastroesophageal reflux disease; 0.4% vs. 34.2% developed sleep apnea; 3% vs. 11.2% developed lipid disorders; and 0.9% vs. 41.9% developed hypertension.
Clearly, the study shows that bariatric surgery is instrumental in preventing the onset of obesity-related illnesses. And that any patients who are denied insurance coverage for weight loss procedures may experience deteriorating health in a fairly short length of time.
This suggests that health insurance carriers should take into consideration more than the current health status of patients who are applying for coverage for bariatric surgery, and that medically eligible patients are risking the onset of health problems that may well develop in the future.
- BARIATRIC ARTICLES & INFO
Life after Weight Loss Surgery
For those that are overweight and have battled countless hours, days, months, and even years of exhausting weight loss efforts, bariatric surgery has become the last…
About Gastric Sleeve
Gastric sleeve surgery is one of the newest innovations in bariatric surgery. The most important thing to know about gastric sleeve surgery is it is typically used for…
Restorative Obesity Surgery
After gastric bypass surgery, about 17% of patients will begin to gain the weight back within five years. This is mostly due to…