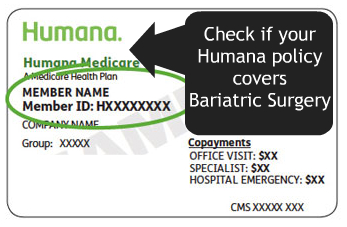
Humana Insurance
What Does Humana Require to Cover Bariatric Insurance
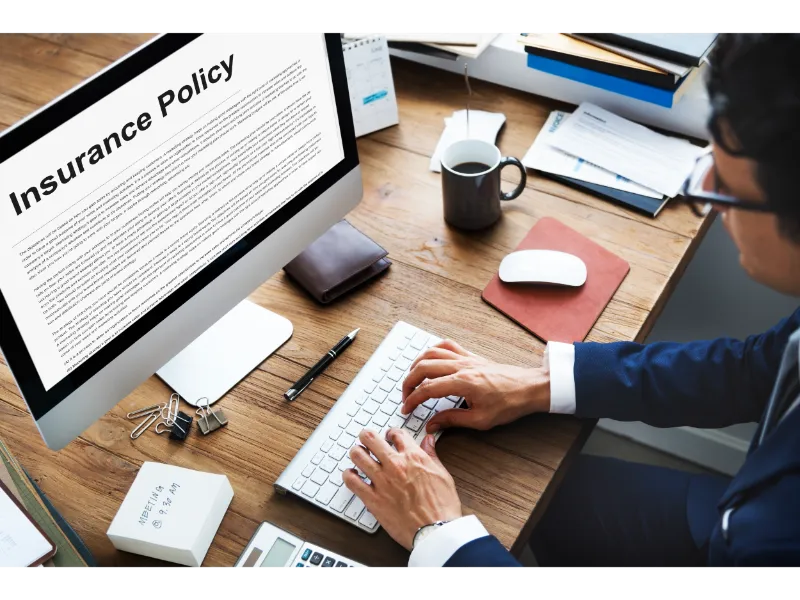
Unless it is stated in your policy, Humana will cover your weight loss surgery. With the help of its Bariatric Management Team, you will be guided through the weight loss surgery and for six months after the surgery.
What Are The Pre-Approval Requirements From Humana
Before Humana approves payment for a weight loss surgery, people must meet the criteria it sets forth, as below:
- 40+ Body Mass Index (BMI)
- 35+ BMI along with any of the four conditions:
- Type 2 Diabetes
- Joint Disease
- Severe Sleep Apnea
- Hypertension
- Primary Care Physician letter that recommends the weight loss surgery
- 18 years old or older
- Six months of doctor-supervised weight loss program
- Patient undergoes and passes the psychological evaluation
What Kinds Of Weight Loss Surgeries Will Humana Cover and What Does It Exclude
- Duodenal Switch Surgery
- Gastric Bypass Surgery
- Gastric Sleeve
- Lap Band (also known as the Realize Band Surgery)
Humana will cover the lap band fills so long as it’s at the in-network providers.
THERE ARE FOUR PROCEDURES THAT HUMANA WILL NOT COVER:
- Gastric Plication (with the gastric band)
- Mini-gastric bypass
- Stomaphyx
- Other investigative procedures
Where Must Patients Go For Surgery?
Humana requires that its policyholders user an accredited Center of Excellence for their surgery and an in-network surgeon.
Should Patients Use The In-Network Bariatric Surgeon?
It is recommended that patients use the in-network Bariatric Surgeon, which will cost less than if they use an out-of-network Bariatric Surgery.
For more information, contact Humana about the weight loss surgery.