Aetna Insurance
What Does Aetna Require Before Insurance Pays For Weight Loss Surgery
When you’re in need of a weight loss surgery and have Aetna as your health coverage, you’ll be glad to know that it covers the majority of the weight loss surgeries. However, Aetna’s HMO and QPOS plans do not include surgical operations for obesity treatment unless prior approval is given by Aetna.
What Does Aetna Require Before Approval Of Bariatric Surgery
If you have Aetna and want to be eligible for the weight loss surgery, you need to meet their criteria listed below:
Adults – 18 years of age or older, must have been considered severely obese for two years (or 24 months), which has been clinically documented. What does it mean to be severely obese?
- Body Mass Index of 40 or more
- BMI of more than 35 along with any of the following health conditions
- Substantial obstructive sleep apnea
- Coronary heart disease
- Medically refractory high blood pressure (140/90 even with using 3 different high blood pressure medications)
- Type 2 diabetes mellitus
Adolescents – Teenagers who have completed their bone growth (age 15 for boys; 13 for girls) are eligible so long as their obesity comes with serious co-conditions.
A 40+ BMI with any three co-conditions:
- Type 2 diabetes mellitus
- Serious obstructive sleep apnea
- Psedotumor comorbidities
A 50+ BMI with one or more of the less serious co-conditions
- Hypertension or medically refractory hypertension
- Nonalcoholic steatohepatitis
- Dyslipidemias
- Serious impairment of daily living
- Venous stasis disease
- Stress urinary incontinence
- Intertriginous soft-tissue infections
- Serious impairment of daily living activities
- Gastroesophageal reflux disease
- Psychosocial distress due to obesity
- Arthropathies due to weight
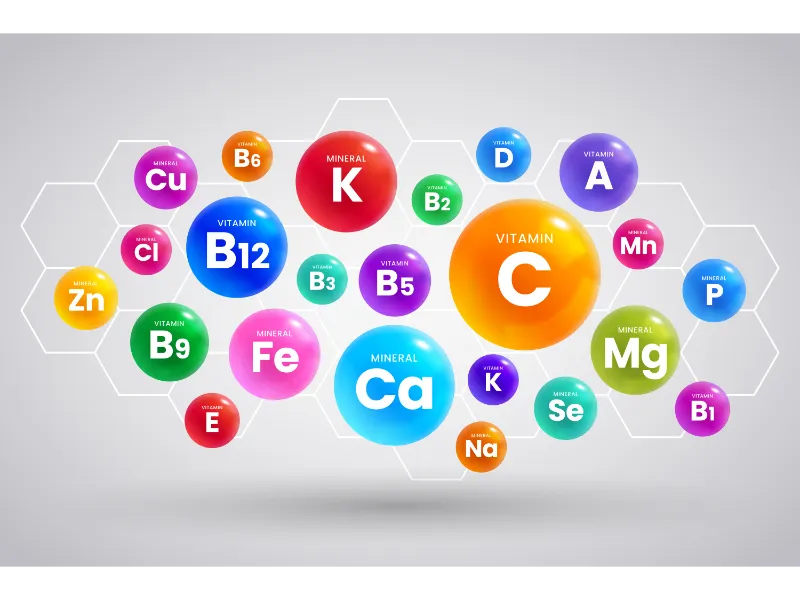
Members who have tried to lose weight in the past but have not successfully had a loss in weight. Members will need to meet either criterion one or two. Patients had to participate in a food and exercise program that has been doctor supervised such as:
- Low calorie diet
- Behavior modification
- Dietician consultation
- Increase of physical activity
All of this must have been recorded in the medical records at every visit.
What does it mean by a doctor-supervised exercise and food program?
- The patient’s participation in the food and exercise program has been doctor-documented in the person’s medical records. An exercise and food program may be given as one part of the before surgical regimen and participation may be surgeon-supervised. A summary letter from a physician does not qualify as satisfactory documentation.
- The documentation must have:
- Doctor’s medical records, noting the progress of the patient throughout the exercise and food program. Patients involved in a physician-given exercise and food program, records that reflect their participation and progress can be an alternative to a doctor’s medical records. A physician will work in correlation with nutritionists and dieticians in the exercise and food program.
- The program must have been used concurrently for six months or more and take place within two years before the surgery with membership in one program for three months. You may be able to certify before you finish the food and exercise program so long as participation in the program has been going on for six months and is done before the surgery date.
OR
- Multi-disciplinary preliminary regimen for surgery:
- Within six months of the surgery, the patient must be partaking in an structured multidisciplinary preliminary regimen for surgery for three months, making sure to follow all the criteria to boost the surgical outcome, lessen the possible complications and establish their ability to deal with and follow all dietary restrictions and post-operative medical care.
- Supervision of behavior modification program by a doctor.
- Dietician consultation.
- Documentation of the participation in the medical records at every visit. A summary letter from the doctor is not enough for documentation. Rather, the documentation needs to include:
- Medical records of doctor’s initial assessment and doctor’s assessment after completion of the regimen.
- Exercise program to improve the pulmonary reserve before surgery and be supervised by a qualified professional or exercise therapist.
- Program must have been done face to face, not remotely.
- A supervised nutritionist diet programs that is reduced in calories.
For people who have a history of psychiatric disturbances – borderline personality disorder, schizophrenia, severe depression, etc. – or are presently under the care of a psychiatrist/psychologist or are using psychotropic drugs, there must be a before-operation psychological approval to ensure patients can comply with the before and after surgery care or can actually consent to the weight loss surgery.
Obesity-causing depression is not a reason for denial for obesity surgery.
Aetna Covers Four Kinds Of Weight Loss Surgeries:
- Duodenal Switch
- Lap Gastric Bands
- Lap Gastric Bypass
- Lap Gastric Sleeve
The following surgeries are not covered by Aetna:
- Bariatric surgery (so long as it’s an idiopathic intracranial hypertension treatment)
- Mini gastric bypass
- Intragastric balloon
- Roux-en-Y gastric bypass (gastroesophageal reflux treatment in people who are not obese)
- Loop gastric bypass
- VBG (except in some circumstances noted above)
- LASGB, RYGB, and BPD/DS procedures (ones that do not meet the above criteria)
- Gastroplasty
- Silastic ring vertical gastric bypass
- Laparoscopic gastric placation
Are Patients Required To Use A Center of Excellence?
Aetna does not make any specification of where the weight loss surgery needs to take place.
Is It Required To Use An In-Network Bariatric Surgeon?
Your policy will dictate the answer; but, if you use the in-network doctor, you won’t pay near as much.
This information may change. To get the most up to date information it is best to contact your insurance or have a bariatric coordinator contact them for you.
Contact Info For Aetna Contact Aetna at 1-800-US-AETNA between 7 a.m. and 7 p.m. or by email at www.aetna.com