How Gastric Bypass Surgery Is Preformed
Performing Gastric Bypass Surgery: How Laparoscopy Works
Gastric Bypass Surgery is the most common Bariatric procedure performed in the U.S., equaling more than 200,000 weight loss surgeries annually in 2008, and that number continues to climb with the use of medical techniques such as Laparoscopy. Laparoscopy Surgery, or limited access surgery, is a predominantly non-invasive technique in which the Bariatric surgeon makes several tiny incisions. One incision allows the entrance of a surgical telescope equipped with a video camera while the other incisions will accommodate the necessary surgical instruments needed to perform the Gastric Bypass.
As a rule, the Bariatric surgeon uses video imaging to conduct a Gastric Bypass, allowing the limited access surgery technique to be used. Limited access surgery offers a two-dimensional look for doctors while limiting the handling and feeling of tissues, providing a less invasive approach and in most cases, faster healing. Bariatric surgery techniques have come a long way. In 1993, the Gastric Bypass (Roux-en-Y) performed by Laparoscopy was considered a highly problematic technique but today Bariatric surgeons rely on this limited access surgery due to a high rate of success and numerous benefits such as:
- Faster recovery time
- Fewer and smaller scars
- Less discomfort
- Decreased hospital stay
- Reduced risk of developing an incisional hernia
Gastric Bypass Surgery: Important Features
Gastric Bypass Surgery is a two-step procedure in which the Bariatric surgeon creates a tiny pouch using only the upper portion of the stomach. Bypassing the rest of the stomach reduces the amount of food that can be consumed and digested. Depending on the surgeon chosen to perform the Bariatric procedure, the stomach may be divided in such a way that it will not return to its previous undivided state. The second step of Gastric Bypass Surgery involves the restructuring of the GI tract, which helps both sections of the stomach drain properly. Below are several additional variations you can expect with Bariatric surgery:
- Altering small intestine lengths
- Amount of food absorption
- Unfavorable dietary effects
Goals of Gastric Bypass Surgery
The Bariatric surgeon’s primary goal is to reduce the size of the stomach by more than 90 percent, therefore reducing its elasticity from more than 1000 mL to an unchanging 15 mL. This is done by creating a pouch from an area of the stomach that is less elastic and not as prone to stretching. Additionally, the original size of the new pouch will prevent any long term changes regarding volume. However, there are two factors that will change with Gastric Bypass Surgery:
- A reduced ability to hold more food in the small intestine
- Decreased connection size regarding the stomach and intestine After Gastric Bypass Surgery, the patient will gradually develop an increase in the pouch’s functional volume but this will not sabotage weight loss, as the Bariatric patient will have already experienced considerable positive results.
How the Pouch Responds to Food
When the Bariatric patient consumes a small bite of food, the body’s first response kicks in, stretching the stomach wall. Nerves within the pouch sends messages of fullness to the brain, allowing the patient to feel as if he has consumed a large meal instead of a few bites. While most people would continue to eat even though they feel full, Bariatric patients quickly learn that any additional bites should be consumed very carefully and slowly to prevent vomiting and discomfort. Once in the pouch, the food is churned with stomach acids, breaking it down before sending it to the small intestine.
Gastric Bypass and the Small Intestine
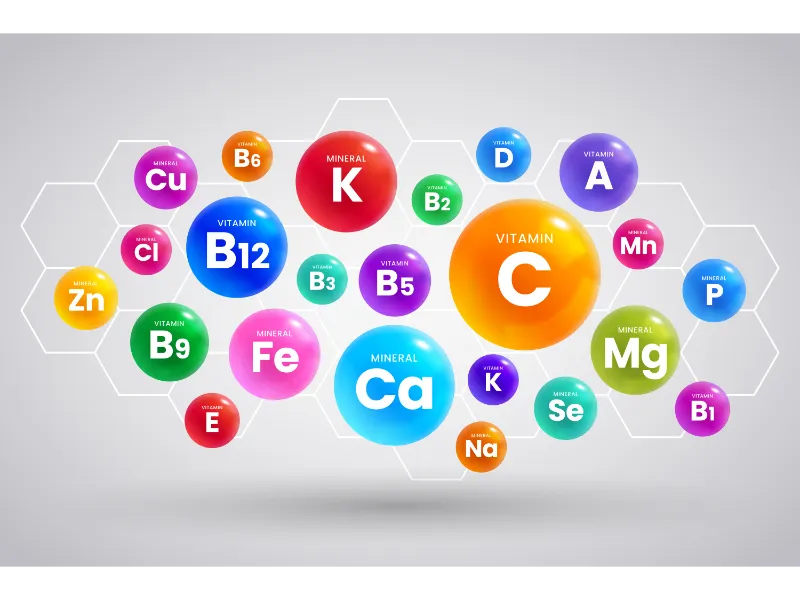
When food is passed from the pouch into the small intestine, the lumen comes in contact with the nutrients. This event causes hormones to be released, hindering any additional food from entering the intestine. Another hormone called Ghrelin is then released within the stomach. This stimulates hunger and another intake of food. While it is not understood why this happens, these and other hormone changes reduce food consumption after Gastric Bypass Surgery. What will happen to the part of the stomach that is bypassed? Most of the time the stomach is left in place with its blood supply intact. Occasionally the lower bypassed part of the stomach it may shrink a bit and its lining (the mucosa) may atrophy. This “left over” part of the stomach will not receive or process food, though it will still contributes to the function of the intestines by absorbing Vitamin B12, and can affect hormone balance and motility of the intestines.
Will my stomach pouch stretch?
The size of your stomach pouch will vary by surgical procedure and surgeon. In the gastric bypass, the stomach pouch is created at one ounce or less in size (15 to 20 cc). Typically after 6 months to a year, the stomach pouch may expand and will become more expandable as swelling subsides. After the first year most patients will end up being able to eat 4-8 oz per meal per day.
What will the staples do inside my abdomen? Are they left there forever?
The surgical staples used on the gastric bypass are extremely tiny in comparison to the staples you use in the office. The Staples are so small that it is difficult to see with the human eye, other than as a tiny bright spot. The staple is made out of stainless steel or titanium. Because titanium and stainless steel are inert in the body, typically do not cause any problems. The staple materials are non-magnetic, so they won’t be affected by a MRI.
Will I just keep losing weight until I waste away? How will I stop losing the weight when I have achieved my goal?
The chances that patients will lose so much weight to the point of malnutrition is very unlikely. 2 things happen to allow weight to stabilize when you are close to your goal weight.
• First, a patient’s ongoing metabolic needs (calories burned) decrease as the body sheds excess pounds.
• Second, there is a natural progressive increase in calorie and nutrient intake over the months following weight-loss surgery. The stomach pouch and attached small intestine learn to work together better, and there is some expansion in pouch size over a period of months.
Proper Eating Behaviors and Gastric Bypass
Gastric Bypass Surgery is a Bariatric procedure that positively affects weight loss by significantly modifying the patient’s eating behavior and tracking weight loss rather than by malabsorption or simple mechanical restriction. To get the most benefits from weight loss surgery, Bariatric patients are advised to eat only during mealtimes. These mealtimes should be scheduled five or six times per day at regular intervals, resisting the urge to snack, or graze, on food throughout the day. Bariatric patients should consume between 80 and 100 grams of protein daily, and when enjoying a meal, always strive to consume their protein rich portions first before having vegetables or carbohydrates. After Gastric Bypass Surgery, meals should be anywhere from ¼ to ½ cup servings. Gradually, this amount will be increased to one cup servings, normally by the end of the first year, allowing the Bariatric patient to make long term changes that become healthy lifelong habits.